How have people in Surrey looked after their wellbeing through the centuries — and what can we learn from them today? That’s the question behind a new year-long heritage and wellbeing initiative backed by the National Lottery.
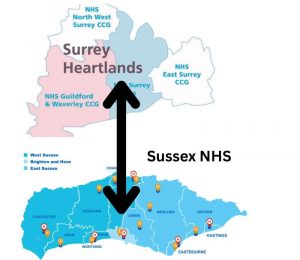
It’s Not Your Birthday But… (INYBB), a Surrey-based arts and social impact organisation, has been awarded £99,781 by The National Lottery Heritage Fund to deliver What Keeps Us Well, in partnership with the Surrey History Centre (SHC). The project runs from August 2025 to July 2026.
Drawing on six miles of historic records held at SHC — ranging from medieval manuscripts to community newsletters — the project will explore how people across Surrey have maintained wellbeing through food, exercise, creativity, connection, and community.
INYBB’s artistic team will collaborate with archivists and three local partner groups to deliver the programme:
- The Halow Project, supporting neurodiverse young people in Guildford and Woking
- Surrey Gypsy Traveller Communities Forum, promoting inclusion and cultural understanding
- Surrey Youth Groups, including LGBTQ+ youth, carers and neurodiverse teens in Woking and Knaphill
Together, they will develop:
- 36 creative workshops
- Training and community events at the Surrey History Centre
- A co-created exhibition showcasing historic sources and new creative responses
- A short documentary film
- A published anthology of written work
- A digital wellness guide
- An open call for artists and writers to create new work inspired by archive material
The project aims to reach over 46,500 people, with a strong emphasis on engaging communities currently underrepresented in heritage activities.
“At a time when mental health challenges are increasing across our communities, this project will highlight how stories from the past can inspire wellness today,” said an INYBB spokesperson.
How to Get Involved
- Volunteers are invited to help with exhibitions, research and more
- Venues (libraries, community centres, health hubs) are encouraged to host the free exhibition
- Artists and writers will be invited to respond creatively to archive materials through an open call launching this autumn
To register interest or find out more, visit itsnotyourbirthdaybut.com or follow @itsnotyourbirthdaybut on social media.
About INYBB
It’s Not Your Birthday But… (INYBB) is a creative organisation working across Surrey and the South East to support wellbeing through arts and social connection. It runs participatory projects that explore identity, place, and belonging — often in partnership with community groups and public bodies. The name reflects the idea that celebration, support and attention shouldn’t be limited to birthdays alone — everyone deserves moments of care and connection, every day.
See HERE more news from the Surrey History Centre
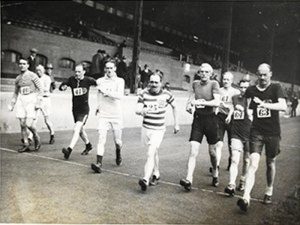
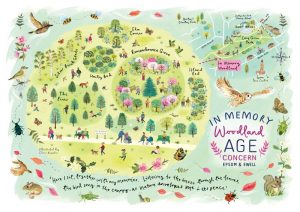
Image: The Centurions group was founded at a meeting of long-distance walking enthusiasts held on 11 May 1911. Courtesy SCC