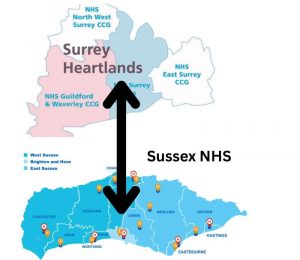
Hundreds of jobs are at risk as two key NHS boards for Sussex and Surrey prepare to merge as part of a money-saving drive by the government. NHS Sussex and NHS Surrey Heartlands – two integrated care boards (ICBs) – are expected to have merged by next April, shedding many of the 1,350 staff who currently work at the two organisations. The changes are part of the latest round of NHS reforms which include the abolition of NHS England and the scrapping of independent patient voice watchdogs known as Healthwatch. Sussex ICB chair Stephen Lightfoot spoke about the forthcoming changes at Brighton and Hove City Council’s Health and Wellbeing Board at Hove Town Hall on Tuesday (22 July).
ICBs bring together NHS organisations, councils and others to plan and commission health services in their area, with the aim of improving health and reducing inequalities. Mr Lightfoot, who will stand down in September, said that ICBs were told in March to halve their running costs – from £39.83 to £18.76 per head of population – by December. Further bad news followed when an analysis of national funding allocations suggested that Sussex was overfunded by £186 million. Mr Lightfoot said that NHS Sussex had a £4.5 billion budget for NHS services in Sussex but the analysis indicated that it should be £4.3 billion and was 4 per cent overfunded. Mr Lightfoot said: “That doesn’t sound a lot on a percentage basis but £200 million is a significant sum of money. Over the next three years, when our demand continues to increase, we’re going to have to reduce our expenditure. We’re going to have to work very hard to make better use of the money that we have.”
He said that this would not affect the budget for delivering healthcare throughout the area – but, he said, combining Sussex and Surrey was the only safe and reliable way to deliver sustainable services. Mr Lightfoot spoke about “the massive scale of this task (and) the huge impact it’s having on our staff … 1,350 people are worried if they’ve got a job. And of course a significant number of them will not have a job in the coming year.” He added: “We’re not alone. The government also confirmed it’s going to rationalise all patient safety regulators. That involves Healthwatch organisations which are going to be closed, not immediately, but over the next 18 months to two years.”
It would be the first time since 1974 that patients would be without a statutory independent voice, the meeting was told.
Sarah Booker-Lewis LDRS