Local women’s health specialist on GTPS
Greater Trochanteric Pain Syndrome (GTPS) is a prevalent condition, particularly affecting peri- and post-menopausal women. It causes significant discomfort in the soft tissue on the outside of the hip and can severely limit mobility. This article discusses the signs, causes, and management of GTPS, with a focus on why it predominantly affects women undergoing hormonal changes.
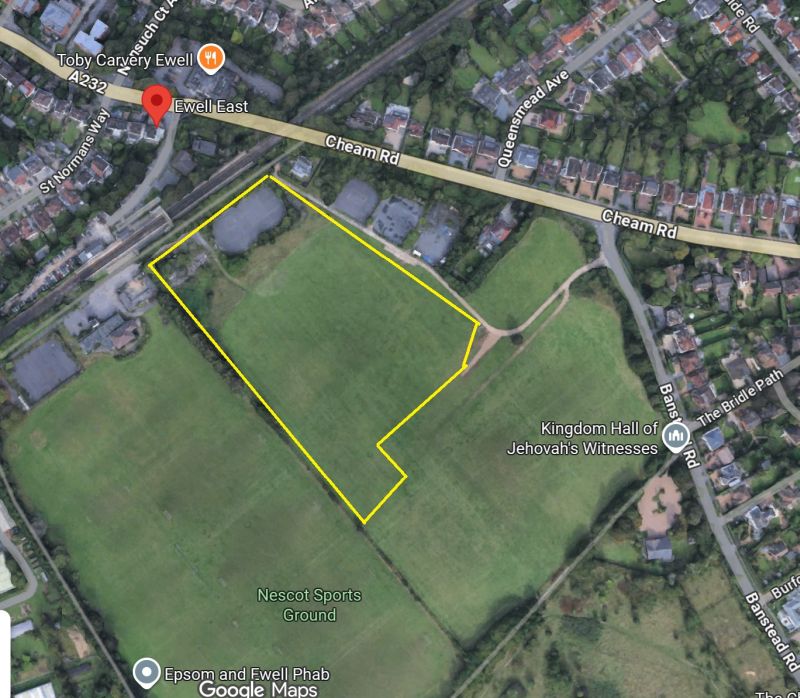
Luke Schembri is an Advanced Physiotherapy Practitioner working within the NHS, while also offering care to a limited number of private patients from his home. Born and raised in Epsom, he has always lived near Epsom Downs, which inspired his initial interest in the horseracing industry where he began his physiotherapy career. Luke is dedicated to delivering evidence-based, high-quality care to his local community. In addition, he authors a fortnightly blog that addresses health and wellbeing topics, particularly aimed at individuals over the age of 40.
What is Greater Trochanteric Pain Syndrome?
GTPS is characterized by pain and tenderness over the greater trochanter, a bony area on the outside of the hip. The condition involves inflammation of the gluteal tendons or bursa, and although it was once called trochanteric bursitis, the term GTPS is now preferred as it covers a broader range of tendon-related disorders.
Signs and Symptoms
The primary symptom of GTPS is pain over the lateral hip, which can radiate down the outer thigh. Key symptoms include:
– Lateral Hip Pain: Often worsened by activities like lying on the affected side, walking, or sitting in low chairs.
– Tenderness Over the Greater Trochanter: Touching this area typically causes discomfort.
– Pain with Activity: Repetitive movements, such as climbing stairs, exacerbate the pain.
– Night Pain: Pain at night is common, particularly when lying on the affected side.
– Weakness or Stiffness: Some may experience hip weakness or stiffness, affecting their gait.
Why is GTPS Most Common in Peri- and Post-Menopausal Women?
GTPS disproportionately affects women in peri- and post-menopause due to hormonal changes and mechanical stress on the hip. Here are the primary reasons:
Hormonal Changes
The decline in oestrogen during menopause impacts the health of tendons, ligaments, and muscles. Oestrogen plays a critical role in maintaining soft tissue integrity, and reduced levels lead to:
– Decreased Collagen Production: Collagen is essential for tendon strength and elasticity, and its decline makes tendons more prone to injury.
– Increased Tendon Stiffness: Lower oestrogen increases tendon stiffness, contributing to gluteal tendinopathies.
– Altered Pain Perception: Hormonal changes during menopause can heighten sensitivity to pain, worsening GTPS symptoms.
Mechanical Load and Changes
Other factors contributing to GTPS in menopausal women include:
– Increased Load on the Hip: Weight gain during menopause places more stress on the hip joints and surrounding tissues.
– Reduced Physical Activity: Lower activity levels can cause muscle weakness, altering hip mechanics and increasing the likelihood of tendon injuries.
– Altered Gait: Pain-induced changes in walking patterns can further strain the hip and lead to GTPS.
Treatment and Management of GTPS
Treatment for GTPS involves conservative methods, physiotherapy, and sometimes more invasive procedures, following the National Institute for Health and Care Excellence (NICE) guidelines, which recommend starting with non-invasive options.
1. Conservative Management
– Rest and Activity Modification: Reducing activities that worsen symptoms, such as standing for long periods or lying on the affected side, is crucial. Using a pillow between the knees when sleeping may help alleviate pressure on the hip.
– Non-Steroidal Anti-Inflammatory Drugs (NSAIDs): These medications can reduce pain and inflammation and are often recommended as initial treatment.
2. Physiotherapy
Physiotherapy plays a key role in treating GTPS and involves:
– Strengthening Exercises: Targeted exercises to strengthen the hip abductors, particularly the gluteus medius and minimus, improve hip stability and reduce strain on the tendons.
– Manual Therapy: Techniques such as deep tissue massage and myofascial release can help relieve muscle tightness and provide short-term pain relief.
– Education and Advice: Physiotherapists offer valuable guidance on managing activities and loading the hip joint to prevent further injury.
3. Shockwave Therapy
Extracorporeal shockwave therapy (ESWT) is a non-invasive option that promotes healing by delivering shockwaves to the affected area. Some studies show positive outcomes for GTPS patients treated with ESWT.
4. Corticosteroid Injections
For patients who do not respond to conservative treatments, corticosteroid injections may be used to reduce inflammation. However, repeated injections can weaken the tendons, so they are not a long-term solution.
5. Surgery
Surgery is rare and reserved for severe cases where other treatments have failed. Options include removing the inflamed bursa or repairing the tendons.
Conclusion
Greater Trochanteric Pain Syndrome is a common condition that primarily affects peri- and post-menopausal women. Hormonal changes and mechanical stress on the hip contribute to its development. Effective treatment usually involves conservative management, physiotherapy, and sometimes shockwave therapy or injections. Early diagnosis and a tailored treatment plan can help alleviate symptoms, improve function, and enhance the quality of life for those affected by GTPS.